Minimally Invasive Spine Surgery (MISS): Future of the Spine Surgery
Spine surgery involves three basic surgeries such as discectomy, decompression and spinal fusion surgery. Discectomy and Decompression surgery relieves pressure put on spinal nerves by removing portions of bone or a herniated disk. The basic idea in Spinal fusion surgery is to take away the painful abnormal movement between spine vertebras by fusing them into a single, solid bone. Spine surgery is traditionally done as "open surgery," meaning the area being operated on is opened with a long incision with significant retraction of the back muscles to allow the surgeon to view and access the anatomy. In recent years, however, technological advances have allowed more back and neck conditions to be treated through small portals avoiding significant damage to the muscles surrounding the spine. In most cases, MISS results in less pain after surgery and a faster recovery.
Procedure
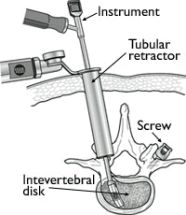
MISS fusions and decompression procedures (such as discectomy and laminectomy) are performed with special tools called tubular retractors. During the procedure, a small incision is made and the tubular retractor is inserted through the skin and soft tissues down to the spinal column. This creates a tunnel to the small area where the problem exists in the spine. The tubular retractor holds the muscles open and is kept in place throughout the procedure. The surgeon accesses the spine using small instruments that fit through the center of the tubular retractor. Any bone or disk material that is removed exits through the retractor, and any devices necessary for fusion such as screws and rods are inserted through the retractor. Some surgeries require more than one retractor
Commonly Performed MISS Procedures
MISS Discectomy-A herniated disk in the lower back that pinches a nerve may cause severe leg pain, numbness, or weakness. To surgical lyrelieve these symptoms, the disk is removed. This procedure is called a discectomy. For the surgery, the patient is positioned face-down and a small incision (< 1 in.) is made over the location of the herniated disk. The surgeon inserts the retractor and removes a small amount of the lamina bone. This provides the surgeon with a view of the spinal nerve and the disk. The surgeon carefully retracts the nerve, removes the damaged disk, and replaces it with bone graft material.
MISS Decompression (Laminotomy)- Indicated in spinal stenosis condition where due to hypertrophy of the ligaments and facet joints the space of the neural canal is compromised. Similar to discectomy with the help of tubular retractors hypertrophied ligament and bone removed to decompress the nerves.
MISS Spinal Fusion- Common procedures performed are MIS Transforaminal lumbar Interbody fusion (MIS TLIF) and MIS Lateral Lumbar Interbody fusion (MIS LLIF). In an MIS TLIF, the patient is positioned face-down and the surgeon places one retractor on either side of the spine. This approach prevents disruption of the midline ligaments and bone. Using the two retractors, the surgeon can remove the lamina and the disk, place the bone graft in to the disk space, and place screws or rods to provide additional support. In MIS LLIF, patient positioned on one side and small incision is made over the lateral abdomen to insert tubular retractors which pass through retroperitoneal area to reach the spine and similarly disc is removed with insertion of the Interbody spacers.
Pros of MISS
Less pain and rapid recovery
Decreased risk of infection
Minimal blood loss
Back muscles are spared to their function
Cons of MISS
Significant learning curve for the surgeon Difficult to perform in multiple levels Significant radiation exposure to patient and surgeon. Most patients who choose MISS vs traditional surgery enjoy earlier return to routine activity with less pain. This means patient can get back to their lifestyle quickly and safely after minimally invasive spine surgery.
Article By
Dr Rahul Chaudhari MBBS MS ECFMG (USA)
Clinical Fellow- Spine/Scoliosis Surgery (USA)
Consultant Spine/Scoliosis Surgeon, Pune